Arden’s Diagnosis: What Does it Mean?
Although I’ve been fairly open about our journey after Arden’s birth, I still get a lot of questions about Arden’s diagnosis and what it means for his medical needs. I don’t mind these questions at all. Arden is our whole world, and we’re proud to share his story of perseverance and resilience with anyone who wants to hear it. As long as questions are asked respectfully, we are happy to answer!
With that said, there are so many different facets of Arden’s journey, that it can sometimes be difficult to create a complete picture of how his journey began, and what his diagnosis will mean as he continues to grow.
Arden was born on April 29, 2020. Although we knew that Arden was breech, we didn’t know what to expect when we were sent to Edmonton one week before his birth for further scans. They suspected possible clubfeet, and there were some concerning measurements found on the ultrasounds that were taken at home. With little to no information on how Arden’s life would look after birth, we traveled to Edmonton on April 22, 2020. Arden and I didn’t leave until almost eight months later.
Soon after Arden was born in Edmonton, we were able to do rapid genetic testing to see what his anomalies might lead to in terms of a diagnosis. Arden was diagnosed with Multiple Pterygium Syndrome, Escobar type, also known as Escobar Syndrome. Arden’s diagnosis is very rare, and unfortunately there are just over fifty documented cases in medical literature. Many of these cases have been documented in third-world countries, where medical intervention is limited. I have had many friends and family members who googled Arden’s syndrome upon hearing the name. Trust me, the google images section of the internet does not paint an accurate or favorable picture of Arden’s unique situation.
Escobar Syndrome is an autosomal recessive condition. Both Brodi and I are carriers for the condition, each having different changes occurring on the same gene, leading to a 25% chance that any children we have will be born with Escobar Syndrome. Of course, we couldn’t have known that before Arden was born.
With Escobar Syndrome, the protein that controls muscle and joint movement in utero does not function appropriately before 33 weeks gestation. After 33 weeks, the ‘adult’ form of that protein takes over, and the muscles and joints are able to move. However, due to weeks of inactivity, the body is left with muscle and joint contractures in almost all limbs. Many children with Escobar Syndrome (including Arden) also have scoliosis, and this was apparent when Arden was born.
Based on an MRI taken during my final week of pregnancy, we knew that Arden would likely need respiratory support after birth, because we could see that his right diaphragm was eventrated. That meant that his diaphragm on that side was positioned way higher than it should have been, which prevented his right lung from fully expanding. At 1 week old, Arden had to undergo diaphragm surgery to correct this. Although his lung expanded, nothing is ever a perfect ‘fix,’ and he still required a lot of breathing support.
Along with all of the visible obstacles that Arden faced, he also had many challenges internally. From the time he was a newborn, Arden had pulmonary hypertension and had to be monitored by the pulmonary hypertension team. This meant that he underwent regular echocardiograms to check that his heart was functioning in partnership with his lungs. With time, Arden outgrew his pulmonary hypertension, which was a relief to us and our team. Arden also developed Ectopic Atrial Tachycardia (E.A.T.). Essentially this means that sometimes his heart rate originates in the wrong part of his heart, causing it to beat way faster than it should. This condition is now well-managed with medication that he takes 3 times per day.
As a newborn, Arden was very stiff – for lack of a better term. His limited movement in utero caused many of his muscles and joints to be very tight. For example, the fingers on his left hand were clenched into a fist and difficult to open, and he held his right wrist at a right angle. His feet were, and still are, positioned differently than typical babies, because he has something called a vertical talus. In simple terms, one of the bones in his right foot is positioned incorrectly, which causes his foot to tip outwards and up. Arden’s legs were, and still are often in a flexed position, and he cannot fully extend them straight (yet).
Respiratory wise, after months of trying extubation (removal of his breathing tube), we were unable to deescalate Arden’s level of respiratory support. Each time they tried to remove his endotracheal tube, it increased the risk of damage when he didn’t tolerate the lack of support, and it needed to be put back in. He was tried on CPAP and BIPAP, both with limited success. Arden did have a BIPAP “scuba mask” for one month, but his respiratory status declined during that time. It was apparent that his body was using far too much energy in order to breathe, making it impossible for him to utilize calories, and grow and develop as needed. In the end our best option was for him to receive a tracheostomy so that he could be provided with long term breathing support with ventilation. Arden underwent his tracheostomy surgery in August 2020, and it was one of our biggest steps towards coming home.
While in hospital, Arden was fed continuously through a nasal-jejunal tube. Essentially, this tube entered through his nose and traveled all the way to his jejunum (the second part of the small intestine). He was fed this way because they wanted all of his energy to be focused on breathing, not on digestion. Because the small intestine does not stretch like the stomach, feeds are given continuously around the clock so that digestion is continuous and doesn’t require large bursts of energy. When it was determined that Arden would need long term breathing support, we also needed to look at long term feeding options. Oral feeding was and still isn’t, possible with his level of ventilation. Therefore, in October of 2020, Arden underwent surgery to place a gastrostomy tube (g-tube). Arden now eats via tube feeding through his g-tube, and he eats at regular intervals throughout the day much like a typical baby.
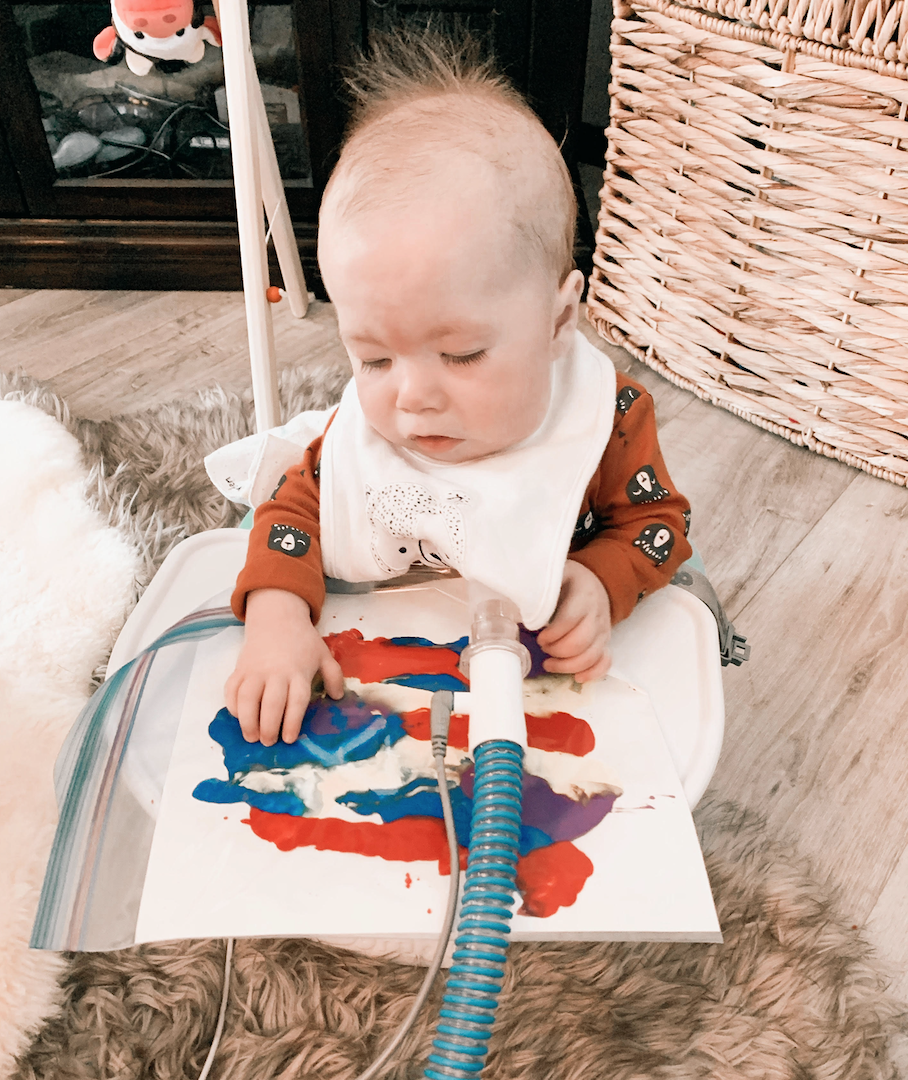
At this point, Arden gets stronger everyday and we have already been able to decrease some of his ventilation support and the amount of oxygen that he requires. As Arden grows, we hope that he will not always need his vent, but only time will tell what his respiratory needs will be. In addition, Arden has come an incredibly long way with gross and fine motor movements. He now has functional range of motion and ability with his arms and hands, and is learning to use his legs more and more.
As Arden grows, he will require various procedures and potentially surgery to help his body achieve its full potential. He may require interventions such as casting, bracing or surgery for his scoliosis. He may require casting and/or surgery to help his legs, ankles and feet achieve functional mobility. He may require long term ventilator support for breathing, or he may be able to come off his ventilator and eventually be decannulated (have his trach removed).
A lot of aspects of Arden’s future are unknown, but we continue to work with many specialists to ensure that all of his medical and developmental needs are met. Physically, Arden has faced and continues to face many challenges. Cognitively, Arden is a typical 9 month old. He’s happy, playful, and enjoys exploring everything in his world. Loving our little man is a full time job, and we celebrate every amazing moment!
XO, Rayel
I love your blog…thinking it will be such an inspiration for many! Arden is such a sweet little guy and you are all so blessed to have such love and support
Thank you so much Janice! We are so lucky to live in such a wonderful community!
This is so informative and such an encouragement to read. Thank you for sharing so candidly.
Thank you so much! I’m glad you enjoyed it!
Thank you for sharing. Your an amazing lady and mother. God choice you to have this amazing little boy, because he knew you had such a big heart. Our prayers and best wishes are with your family. Here is a hug from Brandon.